Living with eczema can be a frustrating experience, especially when it seems like no matter what you do, it just won’t go away. But don’t lose hope just yet! In this article, we will explore effective strategies and tips that can help you finally say goodbye to that pesky eczema for good. Whether you’ve tried countless remedies or are dealing with a recent flare-up, you’ll discover practical solutions that will bring you relief and restore your skin’s health. Say farewell to stubborn eczema and hello to smooth, itch-free skin!
Identifying the underlying cause
External triggers
Eczema, also known as atopic dermatitis, can be triggered by various external factors. These include irritants such as chemicals, soaps, detergents, and certain fabrics. Identifying and avoiding these triggers can help manage and prevent eczema flare-ups.
Internal triggers
Internal triggers, such as stress and anxiety, can also contribute to eczema symptoms. When you are under stress, your body releases certain hormones that can worsen inflammation and lead to eczema flare-ups. Understanding and managing your stress levels can be a crucial part of effectively managing eczema.
Food allergies
Food allergies can also play a role in triggering and exacerbating eczema symptoms. Common allergenic foods include milk, eggs, peanuts, soy, wheat, and fish. Identifying and eliminating these trigger foods from your diet can help alleviate eczema symptoms.
Stress and anxiety
As mentioned earlier, stress and anxiety can have a significant impact on eczema. It is important to find effective ways to manage stress levels, whether through relaxation techniques, therapy, or other stress-reducing activities. This can help decrease the frequency and severity of eczema flare-ups.
Hormonal imbalances
Hormonal imbalances, particularly in women, can influence eczema symptoms. Fluctuations in hormones during the menstrual cycle, pregnancy, or menopause can lead to increased inflammation and eczema flare-ups. Working with a healthcare provider to manage hormonal imbalances can help control eczema symptoms.
Medical treatments
Topical corticosteroids
Topical corticosteroids are commonly prescribed for eczema treatment. These medications help reduce inflammation and relieve itching. They come in various strengths and forms, and your dermatologist will determine the most appropriate option for your specific condition.
Topical calcineurin inhibitors
Another type of topical medication that may be prescribed is calcineurin inhibitors. Unlike corticosteroids, these formulations do not contain steroids and can be used on delicate areas such as the face and groin. They work by suppressing the immune system and reducing inflammation.
Topical immunomodulators
Topical immunomodulators are another option for managing eczema symptoms. These medications modify the immune response, helping to decrease inflammation and alleviate itching. They are often prescribed for moderate to severe eczema that doesn’t respond well to other treatments.
Systemic corticosteroids
In cases of severe eczema, oral or injectable corticosteroids may be prescribed for short-term use. Systemic corticosteroids should be used with caution due to potential side effects, and their use is typically limited to acute flare-ups or when other treatments have failed.
Systemic immunosuppressants
For severe cases of eczema that do not respond well to other treatments, systemic immunosuppressants may be prescribed. These medications suppress the immune system, reducing inflammation and preventing further flare-ups. Regular monitoring and close supervision by a healthcare provider are essential with these medications.
Natural remedies
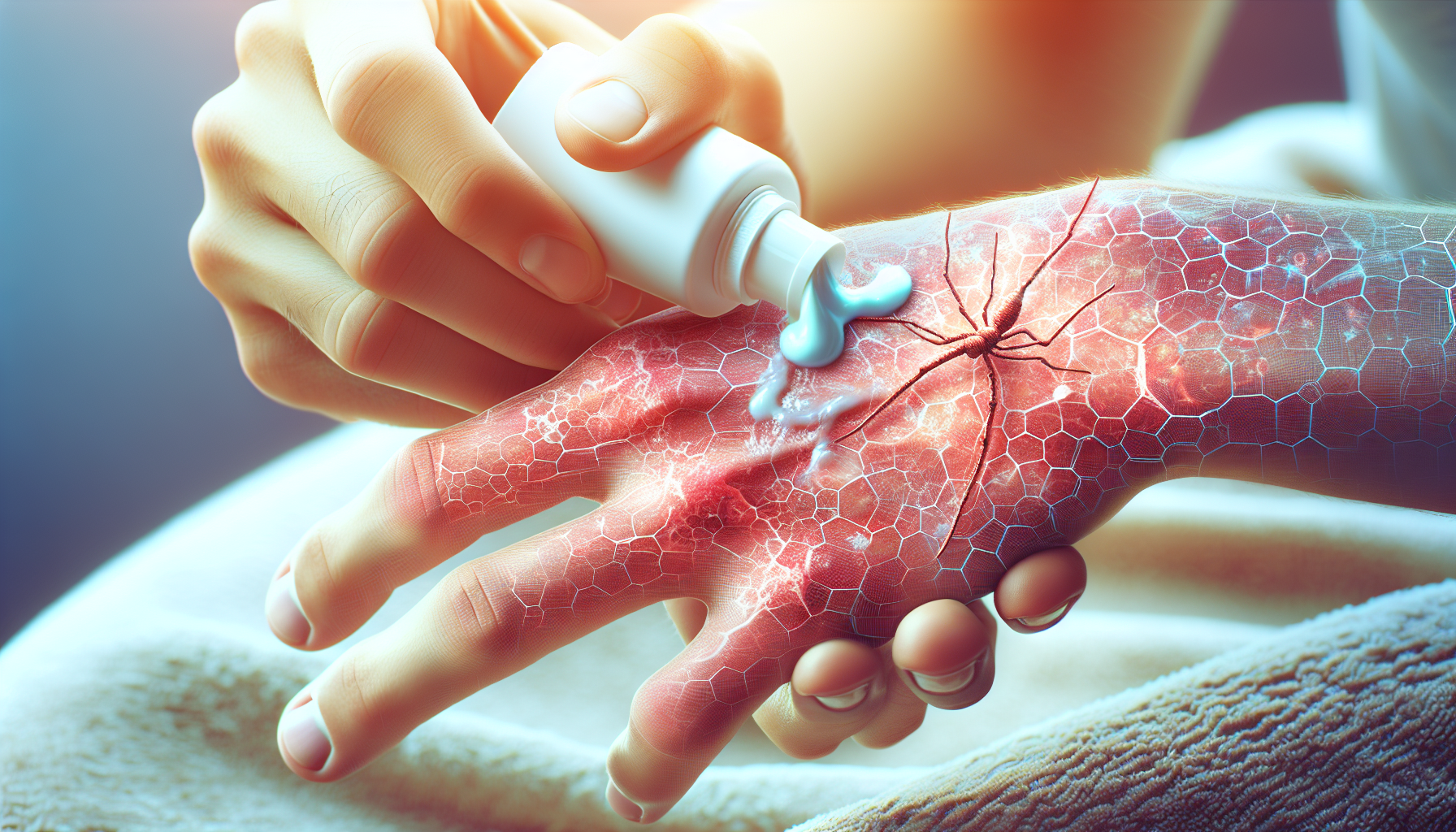
Moisturize regularly
One of the most important aspects of managing and preventing eczema flare-ups is keeping the skin well moisturized. Moisturizers help restore and maintain the skin’s natural barrier function, reducing dryness and itchiness. Opt for fragrance-free moisturizers and apply them generously after bathing or whenever the skin feels dry.
Avoid irritants
To minimize irritation and prevent eczema flare-ups, it is crucial to avoid contact with irritants. This includes harsh soaps, detergents, and cleaning products. Opt for gentle, fragrance-free alternatives, and consider using gloves when handling chemicals or engaging in activities that may irritate the skin.
Use gentle soaps and detergents
Using gentle soaps and detergents is essential in eczema management. Harsh soaps can strip the skin of its natural oils, exacerbating dryness and irritation. Look for mild, fragrance-free cleansers, and avoid excessive scrubbing or hot water, as these can further irritate the skin.
Apply cold compresses
When eczema flare-ups occur, applying cold compresses can help soothe irritated and inflamed skin. Wrap a clean, damp cloth or towel around ice packs and gently apply them to the affected areas. This can provide temporary relief from itching and reduce redness and swelling.
Try wet wrap therapy
Wet wrap therapy involves applying a moisturizer or topical medication to the affected areas and then wrapping them in damp bandages or clothing. This helps lock in moisture and enhances the effectiveness of topical treatments. Consult with a healthcare professional on how to properly perform wet wrap therapy.
Dietary modifications
Identify trigger foods
Identifying trigger foods can be a crucial step in managing eczema through dietary modifications. Keep a food diary to track any patterns between your diet and eczema flare-ups. Common trigger foods include dairy, eggs, gluten, and certain types of nuts or shellfish.
Follow an elimination diet
An elimination diet involves removing potential trigger foods from your diet for a certain period and then gradually reintroducing them to identify any adverse reactions. Consult with a healthcare professional or registered dietitian to design an elimination diet tailored to your specific needs.
Increase intake of anti-inflammatory foods
Incorporating anti-inflammatory foods into your diet can help reduce eczema symptoms. These include fatty fish rich in omega-3 fatty acids, such as salmon and mackerel, as well as fruits, vegetables, whole grains, and healthy fats like avocados and olive oil. These foods can help decrease inflammation in the body.
Consider supplements
Certain supplements may help support skin health and control eczema symptoms. Omega-3 fatty acid supplements, probiotics, and vitamin D supplements are among the options that have shown promise in managing eczema. It is important to consult with a healthcare provider before starting any new supplements.
Lifestyle changes
Manage stress levels
As stress can worsen eczema symptoms, implementing stress management techniques is essential. This can include practices like deep breathing exercises, meditation, yoga, or engaging in hobbies and activities that help you relax and unwind. Finding healthy ways to manage stress can have a positive impact on your eczema.
Practice good skincare habits
Establishing a consistent skincare routine is essential for managing eczema. This includes gentle cleansing, regular moisturizing, and avoiding harsh products. It is important to pat dry instead of rubbing the skin after bathing and to moisturize immediately to lock in moisture.
Avoid hot showers or baths
Hot water can strip the skin of its natural oils and exacerbate eczema symptoms. Instead, opt for lukewarm baths or showers, and limit their duration to 10-15 minutes. Immediately apply a moisturizer after bathing to keep the skin hydrated.
Be cautious with clothing
Choosing the right clothing can help minimize irritation and prevent eczema flare-ups. Opt for soft, breathable fabrics like cotton or bamboo, and avoid synthetic materials or wool that may irritate the skin. Wash new clothes before wearing them to remove any potential irritants.
Maintain a healthy lifestyle
Maintaining a healthy lifestyle can also contribute to managing eczema. Getting regular exercise, eating a balanced diet, staying hydrated, and getting enough quality sleep can support overall skin health and reduce the likelihood of eczema flare-ups.
Alternative treatments
Acupuncture
Acupuncture is a traditional Chinese medicine technique that involves the insertion of thin needles into specific points on the body. Some individuals with eczema have reported positive results from acupuncture, as it may help regulate the body’s energy flow and reduce inflammation.
Herbal remedies
Certain herbal remedies, such as chamomile, calendula, and tea tree oil, have been used topically for their potential anti-inflammatory and soothing properties. However, it is important to consult with a healthcare provider or herbalist before using any herbal remedies, as they may interact with other medications or have their own risks.
Homeopathy
Homeopathy is an alternative treatment approach that uses highly diluted substances to stimulate the body’s innate healing abilities. Some individuals with eczema have found relief through homeopathic remedies tailored to their specific symptoms and constitution. Consult with a qualified homeopath to explore this option.
Ayurveda
Ayurveda is a traditional Indian system of medicine that focuses on achieving balance in the body and mind. Ayurvedic treatments for eczema may involve dietary changes, herbal remedies, and lifestyle modifications. Seek guidance from a qualified Ayurvedic practitioner before pursuing Ayurvedic treatments.
Aromatherapy
Aromatherapy involves the use of essential oils, derived from plants, to promote physical and emotional well-being. While there is limited scientific evidence specifically for eczema, some oils, such as lavender and chamomile, may provide soothing effects when used in skincare products or as part of relaxation techniques.
Preventing flare-ups
Avoid scratching
Avoiding scratching is crucial to prevent eczema flare-ups and worsening of symptoms. Scratching can damage the skin barrier, leading to further irritation and potential infections. Use distraction techniques, apply cold compresses, or use over-the-counter anti-itch creams to alleviate itching instead of scratching.
Keep nails short
Keeping your nails short can help minimize damage to the skin if scratching occurs inadvertently. Long nails can inadvertently break the skin, increasing the risk of infection and further aggravating eczema symptoms. Regularly trim your nails to reduce the potential harm caused by scratching.
Wear breathable fabrics
Choosing clothing made from breathable fabrics, such as cotton or bamboo, can prevent excessive sweating and irritation. These fabrics allow airflow and help to keep the skin dry, reducing the risk of eczema flare-ups. Avoid tight-fitting clothes that can rub against the skin and potentially worsen symptoms.
Use a humidifier
Using a humidifier can help maintain optimal moisture levels in your home, especially during dry seasons or in heated environments. Dry air can worsen eczema symptoms by drying out the skin. A humidifier can add moisture to the air, preventing excessive dryness and reducing the likelihood of flare-ups.
Stay hydrated
Proper hydration is crucial for maintaining healthy skin and preventing eczema flare-ups. Drink sufficient water throughout the day to keep your body hydrated from within. Well-hydrated skin is less prone to dryness and itching. Hydration also helps flush out toxins from the body, promoting overall skin health.
Seeking professional help
Consult with a dermatologist
If your eczema persists and does not respond to at-home remedies or over-the-counter treatments, it is important to seek professional help from a dermatologist. They can assess your condition, provide a proper diagnosis, and recommend an appropriate treatment plan tailored to your specific needs.
Explore allergist consultations
If you suspect that food allergies may be contributing to your eczema, consulting with an allergist can be beneficial. They can conduct allergy tests to identify specific triggers and provide guidance on dietary modifications or allergen avoidance strategies to help manage your eczema effectively.
Consider seeing a psychologist
Eczema can have a significant impact on your emotional well-being, and addressing the psychological aspect is important in comprehensive management. A psychologist or therapist can help you develop coping mechanisms, manage stress, and address any underlying emotional factors that may be exacerbating your eczema.
Join a support group
Connecting with others who have eczema can provide emotional support, shared experiences, and helpful tips. Consider joining a support group, either in person or online, where you can share your journey, learn from others, and receive valuable advice on managing eczema.
Consider alternative therapies
In addition to traditional medical treatments, alternative therapies such as acupuncture, herbal medicine, and homeopathy (mentioned earlier) may be worth exploring. It is important to discuss these options with your healthcare provider to ensure they are safe and appropriate for your individual circumstances.
Long-term management
Develop a skincare routine
Developing a consistent skincare routine is crucial for long-term management of eczema. This includes gentle cleansing, regular moisturizing, and the use of any prescribed topical treatments. Stick to the routine even when your skin is not flaring up to maintain optimal skin health.
Monitor and manage triggers
Continuously monitoring and managing your triggers is essential for long-term eczema management. Keep track of changes in your environment, stress levels, diet, and skincare products to identify any potential triggers. This awareness will help you make necessary adjustments and minimize the risk of flare-ups.
Maintain a healthy lifestyle
A healthy lifestyle, including a balanced diet, regular exercise, adequate sleep, and stress management, can contribute to overall skin health and reduce the frequency and severity of eczema flare-ups. Aim for a holistic approach to health and well-being.
Regularly follow up with healthcare providers
Regular follow-up appointments with your dermatologist, allergist, or any other healthcare providers involved in your eczema management are essential. These check-ins allow for the evaluation of treatment efficacy, the adjustment of treatment plans if necessary, and addressing any concerns or questions you may have.
Adjust treatment plan as needed
Eczema is a dynamic condition, and your treatment plan may need adjustments over time. If your symptoms change, worsen, or do not show improvement, consult with your healthcare provider. They can reassess your condition, explore alternative treatments, or modify existing medications to better manage your eczema.
When to see a doctor
Severe symptoms
If you experience severe eczema symptoms, such as intensely itchy, swollen, or oozing skin, it is important to seek medical attention promptly. Severe symptoms may require stronger medications or additional interventions to provide relief and prevent complications.
Infection
If you notice signs of infection, such as increased pain, warmth, redness, swelling, or pus-like discharge from your eczema-affected skin, it is crucial to see a doctor. Infections can occur when the skin barrier is compromised, and prompt medical treatment is necessary to prevent further complications.
Significant impact on daily life
If eczema significantly impacts your daily life, including your sleep, work, relationships, or emotional well-being, it is important to seek professional help. a healthcare provider can offer guidance and support to improve your quality of life and better manage your eczema.
No improvement after treatment
If you have followed a prescribed treatment plan consistently and have not seen any improvement in your eczema symptoms, it is important to consult with a healthcare provider. They can reassess your condition, potentially conduct further tests, and explore alternative treatment options.
Worsening of symptoms
If your eczema symptoms worsen despite following a prescribed treatment plan, it is important to seek medical advice. Worsening symptoms may indicate the need for adjustments to your treatment regimen or the identification of other factors contributing to your eczema.