Are you curious to know how eczema usually begins? This article aims to provide you with an insightful understanding of the origins of this common skin condition. By exploring the triggers and early symptoms, you will gain valuable knowledge that can help you recognize and address eczema in its early stages, fostering a healthier and more comfortable skin care routine. So, let’s embark on this journey together and uncover how this condition usually kicks off.
What is Eczema
Definition of eczema
Eczema is a chronic skin condition characterized by inflammation and irritation of the skin. It is often accompanied by itching, redness, and the formation of patches or rashes. Eczema can affect individuals of all ages, from infants to adults, and is known to have a genetic component. It is a common condition that affects millions of people worldwide.
Common types of eczema
There are several types of eczema, each with its own distinct characteristics. The most common type is atopic dermatitis, which typically begins in childhood or infancy and is often associated with a family history of allergies or asthma. Other types of eczema include contact dermatitis (caused by exposure to irritants or allergens), nummular eczema (characterized by circular or coin-shaped lesions), and dyshidrotic eczema (affecting the hands and feet and causing blisters).
Prevalence of eczema
Eczema is a widespread skin condition, with studies estimating that it affects up to 20% of children and 3% of adults worldwide. The prevalence of eczema varies across different countries and populations, but it is generally more common in developed countries and urban areas. It is important to note that eczema can have a significant impact on quality of life, resulting in physical discomfort and psychosocial implications for those affected.
Causes of Eczema
Genetic factors
Genetic factors play a significant role in the development of eczema. Individuals with a family history of allergies, asthma, or eczema are more likely to develop the condition themselves. Specific gene variations, such as filaggrin gene mutations, have been linked to an increased risk of eczema. However, it is important to note that genetics alone do not determine whether an individual will develop eczema, as environmental factors also play a crucial role.
Environmental triggers
Various environmental factors can trigger or exacerbate eczema symptoms in susceptible individuals. These triggers can include irritants such as certain soaps, detergents, or harsh chemicals, as well as allergens like pollen, pet dander, or dust mites. Changes in temperature and humidity levels, as well as exposure to certain fabrics or materials, can also contribute to eczema flare-ups.
Immune system dysfunction
Eczema is considered to be an immune system dysfunction, where the immune system overreacts to certain triggers, leading to inflammation and irritation of the skin. In individuals with eczema, the skin barrier is often compromised, making it more susceptible to irritants and allergens. This immune dysregulation can further contribute to the chronic nature of eczema and the recurrence of symptoms.
Symptoms of Eczema
Dry and itchy skin
One of the hallmark symptoms of eczema is dry and itchy skin. Individuals with eczema often experience a constant itchiness or a “itch-scratch cycle” where scratching the skin provides temporary relief but worsens the condition in the long run. The skin may appear rough, scaly, and may even crack or bleed due to excessive scratching.
Red, inflamed patches
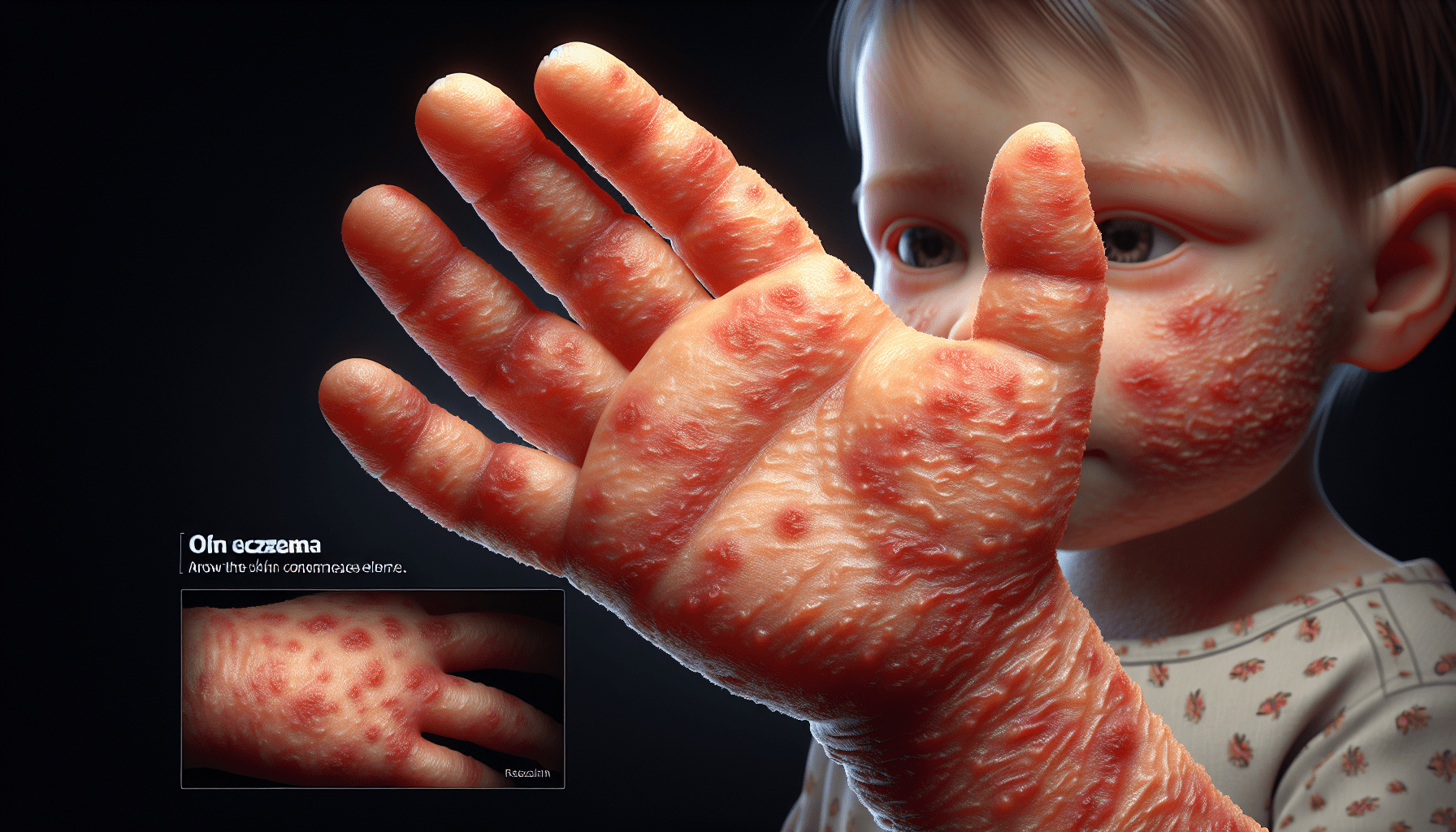
Eczema often presents as red, inflamed patches on the skin. These patches may be itchy, swollen, and warm to the touch. The affected areas may vary in size, from small spots to larger areas of the body. The redness and inflammation are a result of the skin’s immune response to the triggers or irritants.
Skin rash
A common symptom of eczema is the presence of a skin rash. This rash can take different forms and patterns, depending on the type of eczema and its severity. It may appear as raised bumps, blisters, or as dry, scaly patches. The rash can occur on any part of the body but is most commonly found on the face, hands, elbows, and knees.
Crusty or scaly skin
Eczema can cause the skin to become crusty or scaly. This is due to the excessive dryness and shedding of skin cells that often accompany the condition. The affected areas may have a rough texture and may feel rough or rough to the touch. It is important to avoid picking or scratching at these areas, as it can worsen the skin’s condition and lead to further complications.
Blisters or oozing lesions
In certain types of eczema, such as dyshidrotic eczema or allergic contact dermatitis, the skin may develop blisters or oozing lesions. These can be extremely uncomfortable and may cause a burning or stinging sensation. The blisters may eventually burst, leading to oozing or crusting of the affected areas. It is important to seek medical attention if these symptoms occur, as they may require specific treatment.
Eczema and Allergies
The link between eczema and allergies
There is a strong association between eczema and allergies. Many individuals with eczema have a predisposition to develop allergies, as they share a common underlying immune system dysfunction. Having eczema as a child can increase the risk of developing other allergic conditions, such as asthma or allergic rhinitis, later in life. This is known as the “atopic march.”
Common allergens that can trigger eczema
Various allergens can trigger or worsen eczema symptoms in susceptible individuals. These can include common allergens such as pollen, pet dander, dust mites, and certain foods. It is important for individuals with eczema to identify their specific triggers and try to avoid or minimize exposure to them. This can be done through allergy testing and working closely with a healthcare professional.
Testing for allergies in individuals with eczema
When eczema symptoms are severe or difficult to manage, allergy testing may be recommended. This can help identify specific allergens that may be triggering or exacerbating eczema symptoms. Allergy testing methods include skin prick tests, blood tests, and patch tests. By identifying and avoiding allergens, individuals with eczema can better manage their condition and reduce the frequency and severity of flare-ups.
Infantile Eczema
Eczema in infants
Infantile eczema, also known as baby eczema or atopic dermatitis, is a common condition that affects many infants. It usually appears within the first six months of life and can persist into childhood. Infantile eczema often begins on the face and scalp and can spread to other parts of the body. It is characterized by red, itchy patches of skin and may cause discomfort and restlessness in affected infants.
Factors that contribute to infantile eczema
There are several factors that can contribute to the development of infantile eczema. These include a family history of allergies or eczema, a compromised skin barrier, and immune system dysfunction. Additionally, exposure to certain triggers, such as irritants in skincare products or allergens in the environment, can also play a role in triggering or exacerbating infantile eczema.
Treatment options for infantile eczema
The treatment of infantile eczema involves a multifaceted approach aimed at alleviating symptoms and managing the condition effectively. This may include the use of gentle, fragrance-free skincare products, regular moisturization to keep the skin hydrated, avoiding potential triggers and irritants, and addressing underlying allergies if present. In severe cases, topical corticosteroids or other prescription medications may be necessary under the guidance of a healthcare professional.
Childhood and Adolescent Eczema
Eczema during childhood and adolescence
Eczema can persist into childhood and adolescence, causing significant physical and emotional challenges for affected individuals. The symptoms and triggers may be similar to infantile eczema but can vary in severity and location. Eczema during this age group can impact daily activities, sleep, and overall quality of life.
Triggers specific to this age group
Children and adolescents with eczema may have specific triggers that differ from other age groups. These can include factors such as perspiration, certain fabrics or clothing materials, exposure to chlorine in swimming pools, and stress. Identifying and managing these triggers is essential in minimizing flare-ups and ensuring proper management of eczema symptoms.
Impact of eczema on self-esteem and social life
Living with eczema during childhood and adolescence can have a profound impact on an individual’s self-esteem and social life. The visible symptoms of eczema, such as red and inflamed skin or rashes, can lead to self-consciousness, embarrassment, and even bullying from peers. It is important for parents, caregivers, and healthcare professionals to provide emotional support and promote self-acceptance in children and adolescents with eczema.
Management strategies for children and adolescents
Managing eczema in children and adolescents involves a combination of skincare practices, avoidance of triggers, and emotional support. Regular and gentle moisturization, avoiding irritants and allergens, implementing a proper skincare routine, and wearing appropriate clothing can help manage symptoms. Additionally, involvement in support groups or counseling can provide emotional support and coping strategies for children and adolescents with eczema.
Adult-Onset Eczema
Eczema in adulthood
While eczema often starts in childhood or infancy, it can also develop for the first time in adulthood. Adult-onset eczema can be triggered by various factors, including genetics, hormonal changes, environmental irritants, or stress. The symptoms and management of adult-onset eczema are similar to those of childhood or infantile eczema, but the triggers and treatment options may vary.
Common triggers for adult-onset eczema
Adult-onset eczema can be triggered by a range of factors specific to adulthood. These can include hormonal changes, such as during pregnancy or menopause, exposure to certain chemicals or irritants in the workplace, high-stress levels, or even weather changes. Identifying and managing these triggers is crucial in effectively managing adult-onset eczema.
Treatment options and management
The treatment of adult-onset eczema often involves a combination of skincare practices, lifestyle modifications, and medical intervention. Regular moisturization, avoiding triggers, gentle skincare products, and stress management techniques can help alleviate symptoms. Topical corticosteroids, immunomodulators, and other prescription medications may also be necessary in severe cases or when symptoms are difficult to control. It is important to consult with a healthcare professional for proper diagnosis and personalized treatment options.
Eczema Flare-Ups
Factors that can aggravate eczema
Eczema flare-ups can be triggered by various factors, including environmental triggers, skincare products, stress, and lifestyle choices. Exposure to irritants or allergens, changes in temperature or humidity levels, sweating, and certain fabrics or materials can all exacerbate eczema symptoms. Identifying and minimizing these aggravating factors is essential in preventing and managing flare-ups.
Identifying triggers
Identifying triggers for eczema flare-ups often involves keeping a detailed diary of symptoms and potential triggers. This can help individuals pinpoint specific activities, substances, or situations that may be contributing to their eczema. It may be helpful to work closely with a healthcare professional or dermatologist to review these records and develop a personalized management plan.
Preventing and managing flare-ups
Preventing and managing eczema flare-ups requires a proactive approach and a combination of strategies. Avoiding known triggers, practicing good skincare hygiene, keeping the skin adequately moisturized, wearing appropriate clothing, and practicing stress management techniques can all help prevent flare-ups. Additionally, individuals with eczema should follow their prescribed treatment plans and seek medical advice when necessary to effectively manage their condition.
Complications and Associated Conditions
Potential complications of eczema
Eczema, if not properly managed, can lead to various complications. These can include skin infections (due to scratching and breaks in the skin), neurodermatitis (a chronic condition that involves itching and chronic scratching), and sleep disturbances (due to itching and discomfort). In severe cases, the constant scratching and inflammation can cause scarring, changes in skin color, and thickened skin.
Link between eczema and other conditions
Eczema has been found to be associated with other allergic conditions, such as asthma and allergic rhinitis. This shared allergic tendency, known as atopy, suggests a common underlying immune dysfunction. It is essential for individuals with eczema to monitor and manage their overall health, including regular check-ups with healthcare professionals to address any associated conditions and ensure comprehensive care.
Managing comorbidities
Managing associated conditions and comorbidities requires a holistic approach. This may involve working closely with healthcare professionals to develop personalized treatment plans, managing allergies and asthma symptoms, and addressing any underlying triggers that may be contributing to these conditions. Regular follow-ups and adherence to recommended medications and treatment strategies are key to effectively managing comorbidities alongside eczema.
Seeking Medical Help
When to consult a healthcare professional
It is recommended to consult a healthcare professional for proper diagnosis and management of eczema. You should seek medical help if:
- Symptoms are severe or worsening
- Skin infections develop
- There is significant discomfort or pain
- Normal daily activities are affected
- Sleep disturbances occur due to itching or discomfort
- Symptoms persist despite self-care measures
- Emotional well-being is impacted
Diagnosing eczema
The diagnosis of eczema is usually based on a thorough medical history, physical examination, and evaluation of symptoms. Healthcare professionals may also review skin biopsy results or perform allergy testing to assess triggers and associated conditions. It is important to provide detailed information about symptoms, triggers, and any family history of allergies or skin conditions to aid in the diagnosis process.
Treatment options available
Treatment options for eczema aim to alleviate symptoms, reduce inflammation, and prevent flare-ups. These can include:
- Topical corticosteroids or immunomodulators to reduce inflammation
- Moisturizers and emollients to hydrate and protect the skin
- Topical calcineurin inhibitors for sensitive areas
- Oral antihistamines to relieve itching and improve sleep
- Antibiotics for secondary infections
- Phototherapy or light therapy for severe cases
- Systemic medications (such as oral corticosteroids) in severe or resistant cases
It is important to work closely with a healthcare professional to develop a personalized treatment plan based on the severity, triggers, and individual needs of each person.
In conclusion, eczema is a complex and chronic skin condition that can affect individuals of all ages. It involves a combination of genetic factors, environmental triggers, and immune system dysfunction. It is characterized by various symptoms, including dry and itchy skin, redness, rashes, and blisters. Eczema is often associated with allergies and can have significant physical and emotional implications. Management strategies include identifying triggers, proper skincare, lifestyle modifications, and medical intervention when necessary. Seeking medical help and following a comprehensive treatment plan are essential in effectively managing eczema and ensuring optimal quality of life.